How Stress Can Cause Depression: Understanding the Link and Risks Involved
February 20, 2026 | By Mara Sullivan
You have been holding it together for so long that "stressed" feels like your new normal. But lately, the exhaustion runs deeper than just being tired. It is not just about being busy with work or family anymore; it is about feeling empty, detached, or stuck in a mental fog that sleep won't fix. You might be wondering: Is this just burnout, or is it something more serious?
You aren't alone in asking this question. The short answer is yes—chronic stress can cause depression. It isn't a sign of weakness or a lack of willpower; it is a biological reality. When your body's alarm system stays on for too long, it physically alters your brain chemistry, paving the way for depressive disorders.
In this guide, we will explain exactly how stress hijacks your mood, help you distinguish between temporary overwhelm and clinical depression, and provide actionable steps to break the cycle. If you are unsure where you stand right now, you can explore our comprehensive depression screening guide to better understand your current emotional state.
The Biological Link: How Stress Actually Changes Your Brain
To truly understand why stress leads to depression, we need to look under the hood of your nervous system. It is not just "in your head"—it is in your hormones, your neural pathways, and your body's survival mechanisms.
The "Fight or Flight" Mode Gone Wrong
Your body is designed to handle short bursts of stress effectively. When a tiger chases you, your hypothalmus signals your adrenal glands to flood your system with adrenaline and cortisol. This is the "fight or flight" response. It saves your life by sharpening your focus and tensing your muscles for action.
However, in modern life, the "tiger" has been replaced by a demanding boss, a stack of unpaid bills, or constant family conflict. Unlike the tiger, these threats do not go away after ten minutes. Your brain keeps the alarm bell ringing 24/7. This chronic activation is toxic. It wears down your physical systems, leaving you in a state of constant hyperarousal that eventually crashes into exhaustion.
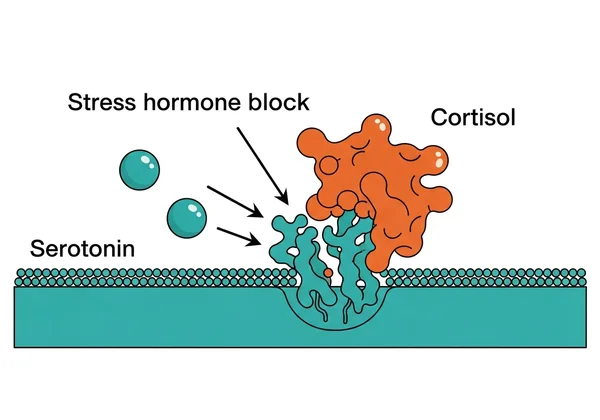
Cortisol's Impact on Serotonin and Dopamine
Cortisol is often called the "stress hormone." In small doses, it regulates energy and inflammation. But when cortisol levels remain high for weeks or months, they become destructive to the brain. High levels of cortisol can actually shrink the hippocampus—the part of the brain responsible for memory and emotion regulation.
More critically, chronic cortisol exposure disrupts the production of serotonin and dopamine—the "feel-good" chemicals responsible for happiness, motivation, and sleep. Think of your brain's chemical balance like a battery. Chronic stress drains the battery faster than it can recharge. Eventually, the battery dies. When your serotonin levels bottom out, you lose the biological ability to feel joy or hope. That is the chemical definition of depression.
Neuroplasticity: Can the Brain Heal?
Here is the good news: the brain is "plastic," meaning it can change and adapt throughout your life. Just as chronic stress can rewire your brain for depression, changing your environment and habits can rewire it back for resilience. This concept, called neuroplasticity, means the damage is not permanent. With the right interventions—like rest, therapy, or lifestyle changes—you can rebuild those depleted pathways and restore your chemical balance.
Am I Stressed or Depressed? Key Differences to Watch
It is easy to confuse the two because they often overlap. You might feel "stressed and depressed" at the same time. However, spotting the biological difference is critical for knowing how to treat it effectively.
Symptoms Unique to Stress (Hyperarousal)
Stress is usually characterized by too much:
- Too much tension: You feel "wired," anxious, or unable to sit still.
- Racing thoughts: Your mind won't shut off, especially at night when you try to sleep.
- Irritability: You might snap at people easily or feel constantly on edge.
- Reaction to logic: If the specific stressor (e.g., the big project at work) disappears, you typically feel instant relief and your mood lifts.
Symptoms Unique to Depression (Numbness)
Depression is often characterized by too little:
- Too little emotion: You feel numb, empty, or "flat." The world seems gray.
- Slowed thoughts: It feels like wading through molasses; even simple decisions like what to eat feel impossible.
- Apathy: You don't care about things that used to matter. Hobbies bring no joy.
- No reaction to logic: Even if the stressor disappears, the dark cloud remains. You feel sad without a specific, tangible reason.
The "Overlap Zone": Stress, Anxiety, and Depression Combined
Ideally, these conditions would stay in their own lanes. In reality, they often crash into each other. You might feel "wired but tired"—anxious energy combined with deep hopelessness. This is common when chronic stress triggers both anxiety and depression simultaneously. Recognizing this mixed state is the first step toward untangling it.
5 Warning Signs That Stress Has Turned into Depression
Transitioning from "stressed out" to "depressed" doesn't happen overnight. It is a slow, often invisible slide. Watch for these five red flags that suggest you've crossed the line from burnout into a depressive disorder.

1. The Stressor Is Gone, But the Mood Remains
Imagine you finally finish that huge deadline or resolve a conflict. You should feel relief, right? If the stressor is gone but you still feel hopeless, exhausted, or empty, that is a major warning sign. Stress is situational; depression is pervasive. It sticks around even when life gets "easier."
2. You’ve Lost Interest in Things You Used to Love
This symptom, clinically called anhedonia, is a hallmark of depression. If your favorite hobby, food, or spending time with friends simply feels like "work" or brings you zero pleasure, your serotonin system is unresponsive. You aren't just "too busy" for fun; you are physically unable to enjoy it.
3. Your Sleep Patterns Are Disrupted
Stress often keeps you awake (insomnia) because your mind is racing. Depression can do that too, but it often flips the switch: you might want to sleep 12 hours a day and still wake up tired. Or, you might wake up at 4 AM every morning unable to fall back asleep (terminal insomnia). If sleep feels like an escape rather than rest, pay attention.
4. You Feel Worthless or Guilt-Ridden
Stress makes you feel overwhelmed ("I can't handle this"). Depression makes you feel worthless ("I am a failure for not handling this"). If your inner critic has turned vicious and personal, attacking your character instead of just your workload, depression is likely speaking.
5. Physical Symptoms Won't Go Away
Unexplained back pain, chronic headaches, digestive issues, or a feeling of "heaviness" in your limbs are common somatic symptoms of depression. Stress causes muscle tension; depression causes a feeling of physical collapse. Your body is shouting what your mind might be ignoring.
Identifying Your Triggers: Common Risks
Why do some people handle pressure while others develop depression? It often comes down to the specific type of stressor and your personal "load."
Situational Triggers: Work, Finances, and Academic Pressure
- Workplace Burnout: High demands coupled with low control (like micromanagement) is a top predictor of depression. It strips away your sense of agency.
- Financial Stress: The constant low-level panic of "making ends meet" keeps cortisol chronically elevated, making it one of the most toxic forms of stress.
- Academic Pressure: For students, the fear of failure can link self-worth entirely to grades, creating a fragile mental state where one bad test feels like the end of the world.
Internal Triggers: Perfectionism and Lack of Control
It’s not just what happens to you; it’s how you interpret it. If you believe "I must be perfect to be loved" or "I have no control over my life," you are biologically more vulnerable to the stress-depression cycle. Perfectionism is a recipe for constant failure in your own eyes, which fuels depression.
Biological Vulnerabilities
Genetics play a huge role. If depression runs in your family, your "stress threshold"—the point at which stress tips into depression—might be lower than others. This isn't your fault; it's your biology. Knowing this can help you take preventative steps earlier.
How to Measure Your Severity Levels Safely
If you are nodding along to these symptoms, you might be feeling anxious about "how bad" it is. Uncertainty breeds fear. Replacing that uncertainty with data can be incredibly empowering and help you decide your next move.
Why Self-Reflection is the First Step
You cannot fix what you do not acknowledge. Keeping a journal or tracking your mood can help, but sometimes you need an objective baseline. Seeing your feelings quantified can validate that what you are experiencing is real and worthy of attention.
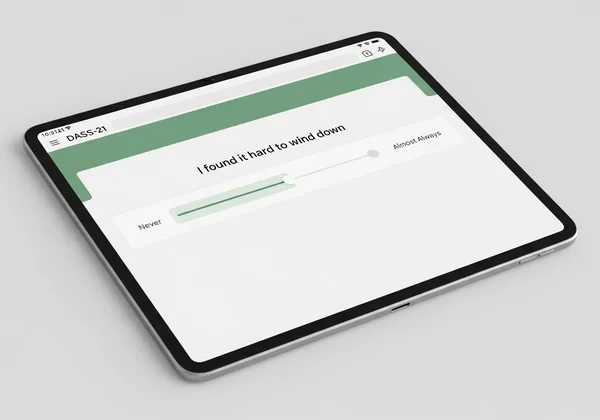
Introducing the DASS-21: A Scientifically Validated Scale
The Depression Anxiety Stress Scales (DASS-21) is a widely recognized tool used by researchers and clinicians globally. It doesn't just give you one label; it separates your symptoms into three distinct buckets: depression, anxiety, and stress. This clarity helps you see, for example, that your "depression" might actually be severe stress, or vice-versa.
What Your Score Can (and Can't) Tell You
A self-assessment is not a medical diagnosis. It is a screening tool for insight.
- It CAN: Tell you if your symptoms are in the "Normal," "Moderate," or "Severe" range compared to the general population.
- It CAN’T: Tell you why you are depressed or prescribe medication.
To get a clearer picture of where you stand today, you can check your traits with this DASS-21 online test. It is free, private, and takes about three minutes to complete.
Breaking the Cycle: Practical Steps to Recovery
Recovery is possible. The goal is to send a "safety signal" to your brain to turn off the cortisol alarm and allow your neurochemistry to reset.
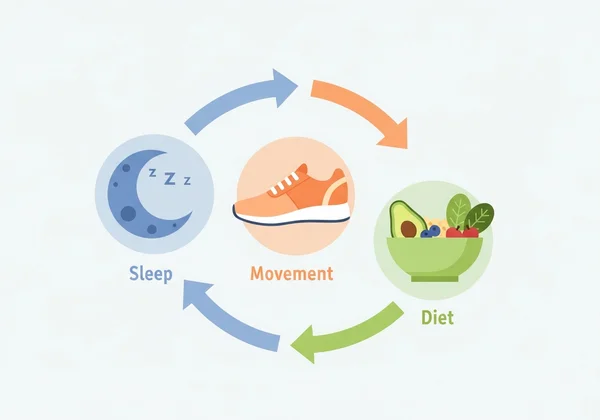
Lifestyle "Medicine": Sleep, Diet, and Movement
- Movement: Exercise is a natural antidepressant. It burns off excess adrenaline and releases endorphins. A 20-minute brisk walk counts. You don't need to run a marathon; you just need to move your body.
- Sleep Hygiene: Protect your sleep at all costs. It is when your brain repairs neurochemistry. Create a "wind-down" routine that starts an hour before bed—no screens, dim lights.
- Diet: Reduce sugar and caffeine, which can mimic anxiety symptoms in the body (jitteriness, racing heart). Focus on whole foods that stabilize your blood sugar.
Cognitive Reframing
Stress is often fueled by "catastrophizing"—assuming the worst possible outcome will happen. Cognitive Behavioral Therapy (CBT) techniques can help you catch these thoughts and challenge them. Ask yourself: Is this thought a fact, or just a fear? What is the evidence for this thought?
Mindfulness and Relaxation
You don't have to become a monk or meditate for an hour. Simple "grounding" exercises—like focusing on your breath for 60 seconds or naming five things you can see—can physically lower your heart rate and interrupt the stress response. Doing this multiple times a day keeps your baseline stress lower.
When to Seek Professional Help
Self-help has limits. If your depression is "severe" on a scale like the DASS-21, or if you are experiencing the following red flags, please seek professional support immediately.
Red Flags Requiring Immediate Attention
- Thoughts of death, suicide, or self-harm.
- Inability to function: You can't get out of bed, shower, or go to work.
- Psychotic symptoms: Hearing voices or seeing things others don't.
- Substance use: Using drugs or alcohol to unwantedly numb the pain.
Professional Treatment Options
Therapy (like CBT) is the gold standard for treating stress-induced depression. It gives you tools to manage the triggers. Medication (antidepressants) can also provide the "floor" you need to stand on while you build your coping skills. There is no shame in using every tool available to you to get better.
Conclusion: Taking Control of Your Mental Health
Can stress cause depression? Yes. But it is not a life sentence. It is a signal from your body that something needs to change. By understanding the link between your environment, your stress hormones, and your mood, you can start to dismantle the cycle.
Recovery starts with awareness. Validate your feelings, prioritize your recovery, and don't be afraid to measure your progress. Take the first step today and try the DASS-21 assessment to gain clarity and regain control of your mental well-being.
Frequently Asked Questions
Can stress and anxiety cause depression together?
Yes, this is extremely common. Chronic stress often triggers anxiety first (the "revved up" phase), which eventually leads to burnout and depression (the "shut down" phase). Tools like the DASS-21 are designed specifically to measure all three conditions simultaneously to untangle this overlap.
Is stress-induced depression permanent?
No. Depression caused by stress is often situational. Once the stressor is removed and the brain has time to heal (neuroplasticity), symptoms usually improve significantly. However, without intervention, it can become chronic, so taking action early is important to prevent long-term patterns.
Can I recover without medication?
Many people with mild to moderate stress-induced depression recover through lifestyle changes, therapy, and stress management alone. However, severe cases often benefit from medication to rebalance brain chemistry enough to make those lifestyle changes possible. Consult a doctor to decide what is right for you.
How long does it take to recover?
It varies by individual. Some people feel relief within weeks of removing the major stressor; for others, it takes months of therapy and lifestyle adjustment. The key is consistency in sending "safety signals" to your brain through rest, boundaries, and self-care.